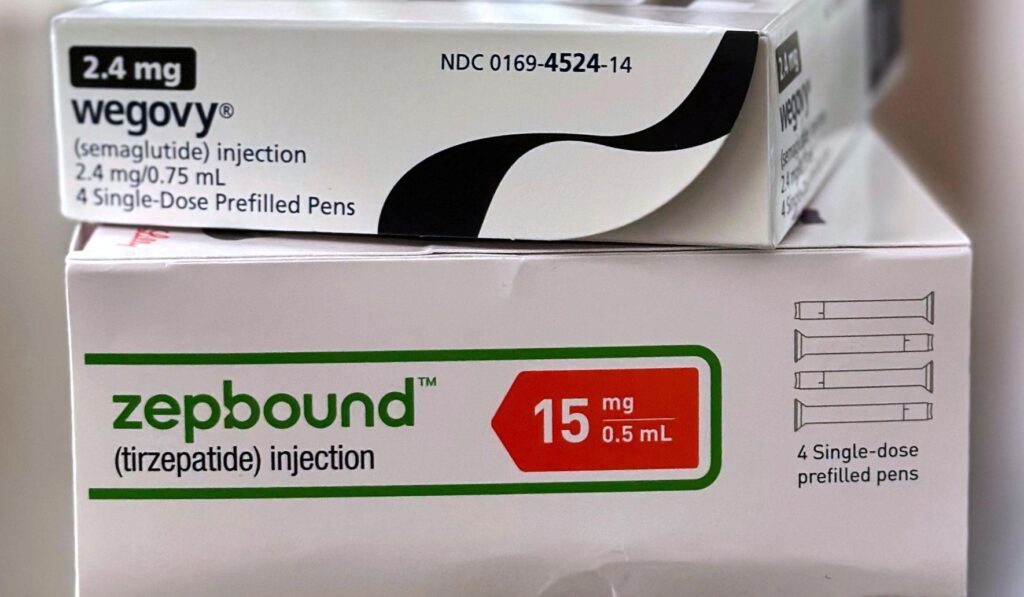
The Trump administration announced a deal Thursday with drugmakers Eli Lilly and Novo Nordisk to lower the prices of their obesity drugs. This move shifts the conversation from blame to results: a White House willing to sit down with private sector players and drive real cost relief. It also raises practical questions about access, competition, and the market signals this deal sends to patients and insurers.
The Trump administration announced a deal Thursday with drugmakers Eli Lilly and Novo Nordisk to lower the prices of their obesity drugs. That exact announcement landed as a clear, public-facing negotiation between government and industry. For people paying out of pocket or watching premiums climb, any promise of lower cost is a welcome development.
Obesity medications have become a major line item in healthcare conversations because they can be expensive and have seen sharp demand. Insurers, employers, and patients have felt the pinch when new, effective therapies hit the market at high prices. Bringing those prices down can ease pressure on families and health plans without shutting down innovation.
A Republican approach to this kind of issue looks for practical steps that preserve market incentives while delivering relief where it matters. Sitting down and cutting a deal with manufacturers respects private investment in research while using negotiating leverage to protect consumers. That balance is exactly what voters expect: results, not grandstanding.
Lower prices open the door to broader access for people who need these treatments but can’t afford them today. When costs fall, doctors can prescribe without worrying whether patients can fill the script. That translates to real health outcomes, fewer complications, and lower downstream spending on conditions linked to obesity.
At the same time, price reductions have to be sustainable so companies keep developing new therapies. If pricing squeezes out margin entirely, it risks dampening investment in the next generation of treatments. Smart deals find room for both patient access and continued private-sector innovation.
The deal also shifts pressure onto competitors and payers to act. When two major manufacturers agree to adjust pricing, it creates market signals that other firms and insurers can’t ignore. That competitive ripple effect can benefit more patients than the initial agreement alone.
Critics will predictably paint any policy engagement as ideological theater, but the practical test is simple: do patients pay less and do more people get treated? Republicans should insist on measurable results and transparent terms so taxpayers and consumers know the real impact. Accountability matters more than slogans.
Employers and health plans will be watching closely to see how savings are passed along. If negotiated reductions are captured at the pharmacy counter, workers see immediate relief. If savings are eaten up by middlemen or administrative costs, the intended benefits vanish before they reach families.
Another factor is how the deal affects long-term affordability and competition. The best outcomes come when negotiated pricing coexists with policies that encourage new entrants and generics. Preserving competition prevents any single company from permanently controlling prices in a way that harms patients down the road.
Regulatory clarity also matters because unclear rules can slow access even when prices drop. Streamlined pathways for approval, clear guidance for prescribing, and predictable reimbursement policies let clinicians adopt new treatments faster. That’s the kind of no-nonsense stewardship conservative voters approve of: efficient government that removes obstacles rather than adds bureaucracy.
Transparency about the terms of the agreement will be critical to public trust. Citizens deserve to know how any discounts are structured, whether rebates flow through insurers, and how patients are protected from misleading billing. Open books and measurable benchmarks turn a political win into a durable policy success.
There will be more negotiating ahead, not just with drugmakers but with insurers, pharmacy benefit managers, and employers. Each group has a role in making prices meaningful at the point of care. Continued engagement will test whether this deal is a one-off headline or the start of a pattern that delivers sustained relief.
Ultimately, the best conservative response is pragmatic and results-driven: encourage private innovation, use government leverage to lower costs, and insist on clear, enforceable terms so patients benefit. If this agreement produces lower out-of-pocket costs and wider access without killing future research, it will be a win for common-sense policy. The next challenge is ensuring those savings actually reach the people who need them most.